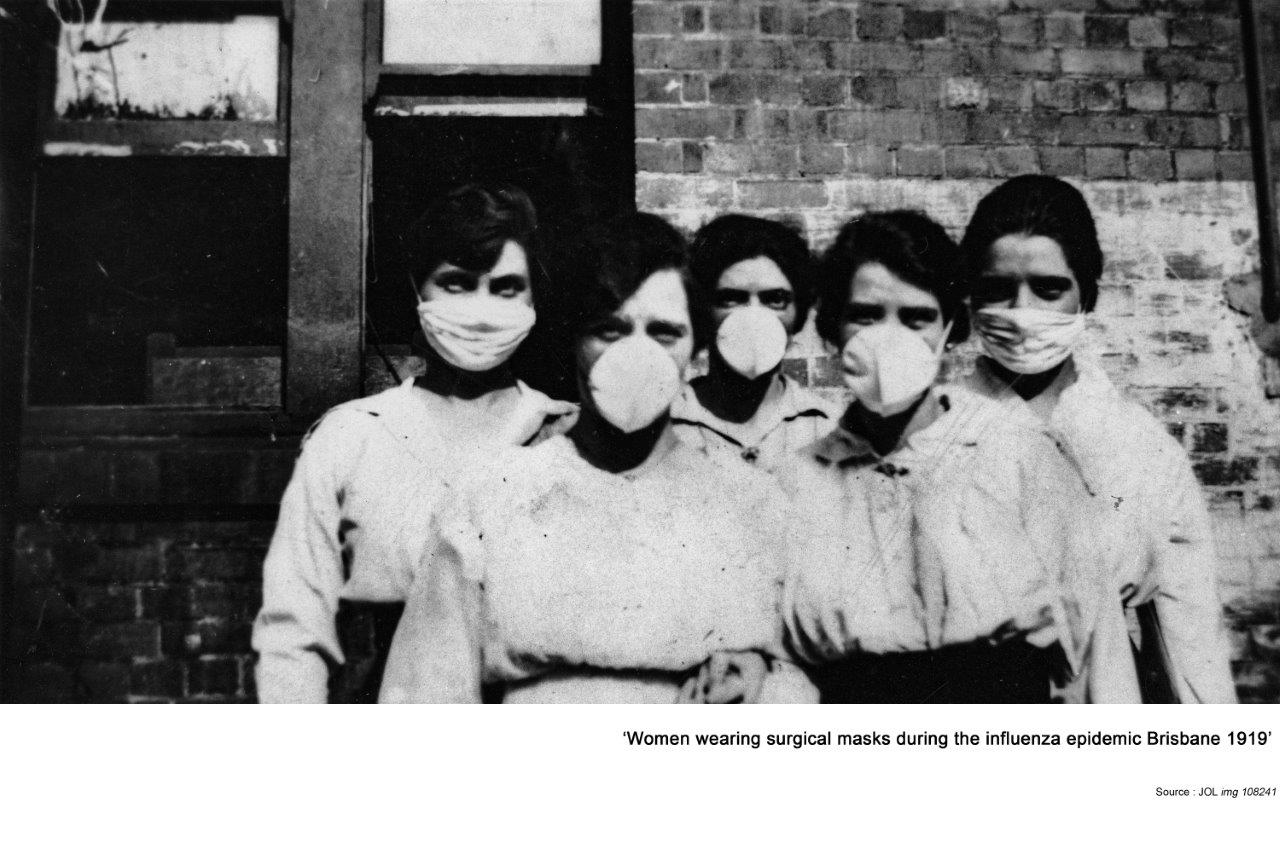
Influenza pandemic 1919
One hundred years ago, an influenza pandemic with a 10-20% mortality rate swept the world following The Great War and caused the death of an estimated 50 to 100m people, or about 5% of the world’s population at the time. This is a summary of the reports concerning influenza in the Medical Journal of Australia (MJA) from 1918 to 1920.
During the war little information had been released for fear of causing despondency. In the public health reports figures for influenza were not published until early 1919, though reference was made to measures put in place in 1915, especially the wearing of masks at public gatherings and the possibility of expired droplets as the most common form of transmission. However, the disease was not mentioned in the MJA through 1916, 1917 and well into 1918. Although the origin and date of the pandemic is unknown, cases had been rising on the Western front for a while and when an outbreak in Spain coincided with the reporting of the illness in the winter of 1918/19, the term Spanish Flu appeared. A mild outbreak in Lithgow, NSW, was identified in 1918 but transmission in Victoria seems to have already been well established so it is presumed that Melbourne, as the main port of entry for returning troops, was the likely starting point in Australia. The virulence and diminished seasonality have never been explained but physical exertion, poor hygiene, inadequate nutrition and high stress levels were likely factors, but the possibly of mutation to new viral types cannot be excluded.
A scientific meeting in March 1920 reported a contemporary view of the pandemic. It was still assumed that disease had a bacteriological origin. Pressor agents, digitalis, pituitary extract, salicylates and alcohol had all been tried and found useless, sometimes exacerbating the condition. There was acknowledgement of a filter-passing agent, but some thought it was derived from fragmented bacteria. Acquired immunity from an infection was short-lived. However, a trial of administering serum from convalescent cases reduced mortality to 6.4% in the most severely affected (when death was the likely outcome). Pneumococcal antiserum had a variable beneficial effect in some studies, but the only consistently useful treatment was found to be rest from physical activity, adequate nutrition and good nursing care. Various prevention measures were tried: Prophylactic repeated convalescent anti-serum and pneumococcal immunisation seemed to offer some help. There were reports that Eucalyptus or zinc sulphate inhalation was beneficial but were not replicable. Isolation measures failed and the risk of excessive consumption of limited resources of funds, staff and materials was recognised, if they were diverted from a simple but proven treatment. By the end of 1919 the pandemic had burnt itself out but neither effective immunisation nor specific remedy had been developed. It became clear that secondary bacterial infection (mainly pulmonary) was the prime cause of morbidity and mortality and extreme contagion meant isolation would not be viable for community protection.
My conclusion was that the pandemic was a facilitating factor in the investigation of viruses, and the progress that these pioneer health professionals made in understanding the problem are truly remarkable considering their ignorance of the pathology involved and the extremely limited pharmacopoeia, laboratory services and treatment facilities available to them. Even with our current knowledge, the problem facing health authorities in the face of a similar pandemic are not so very different, especially if it occurred at a time of massive international disruption, drained human and material resources and a severely stressed population. It may not be the virulence of the infection that we should fear but more our capacity to meet such a catastrophe.