Dr Amy McCart Reed, a molecular genetics specialist at the UQ Centre for Clinical Research, Molecular Breast Pathology group explains the role genetics play in breast cancer.
Breast cancer is now the most commonly diagnosed cancer in Australia, with 1 in 7 women diagnosed in their lifetime. Of all the breast cancers diagnosed, only 5-10 per cent of these are hereditary or ‘familial’ breast cancers, where a genetic change is passed down through families. The rest are referred to as ‘sporadic’ breast cancers.
In familial breast cancers, genetic changes which result in breast cancer can be passed down through both the mother and father. Patients suspected of having a familial breast cancer will be directed for a genetic test. This kind of test will investigate the DNA from the patient’s blood to see if any genetic changes are present in the most common ‘breast cancer genes’, BRCA1 and BRCA2. Although these two genes are the most well-known in familial breast cancer, changes in these genes account for only 15 per cent of all the inherited cancers. Even if a patient has a clear family history, a genetic test may not give a clear answer.
But what about the rest of the breast cancers? Are they genetic too?
Yes. Even if breast cancer is not inherited, it is a genetic disease. Over time, a series of genetic changes accumulate that permit a cell to push through normal checkpoints and divide and develop into cancer. The study of all the types of DNA changes in a cancer cell is called cancer genomics. Genome refers to the complete set of DNA within an organism. Cancer genomics is now at the forefront of breast cancer research, and is essential as we move cancer care towards precision oncology.
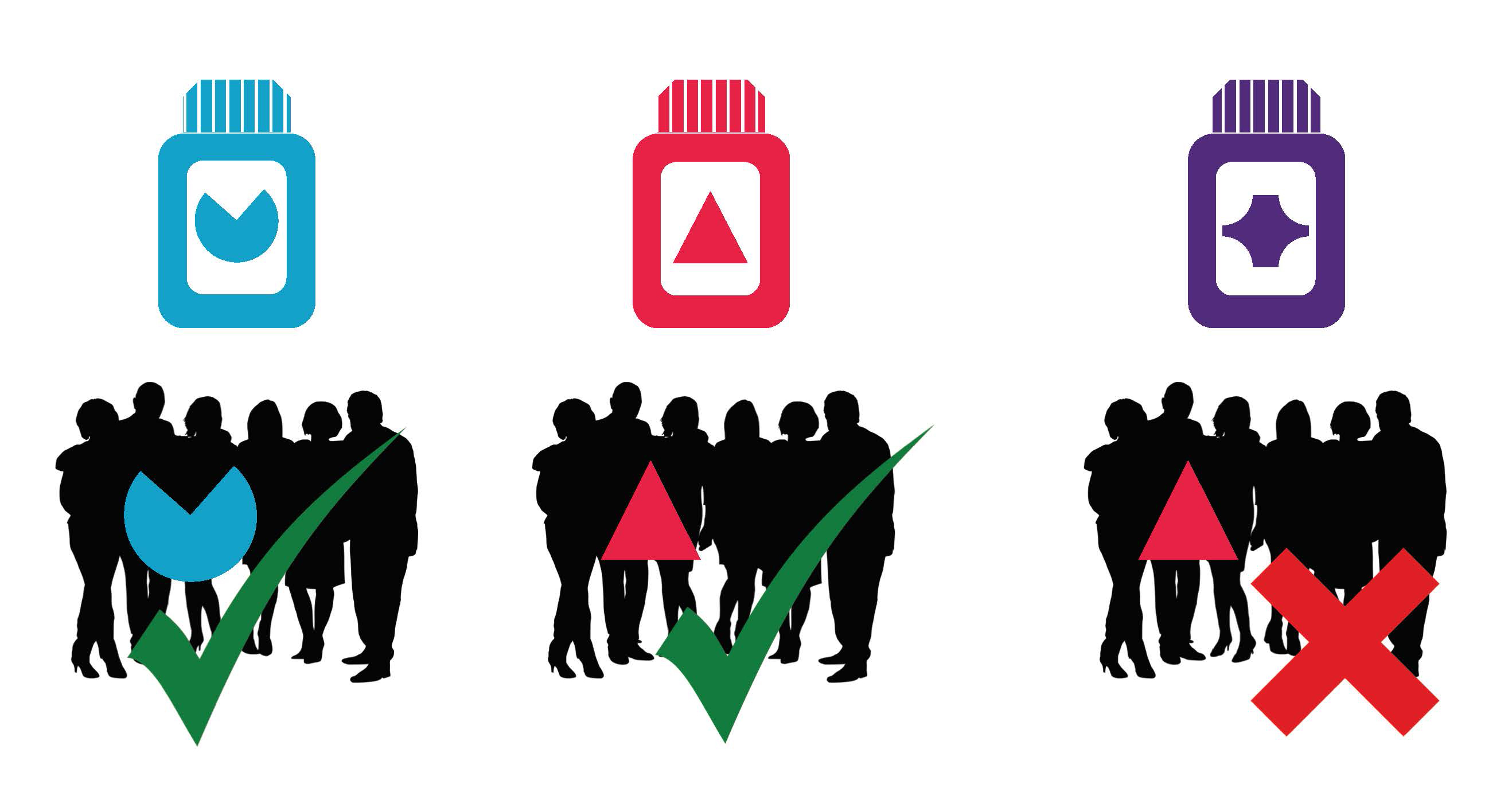
In the very near future, we hope to be able to sequence a patient’s blood DNA and their tumour DNA and work out what changes are specific to the tumour. We can then see if there are particular drugs available that target that specific change. This personalisation is the ideal clinical situation, as some cancer drugs have undesirable side-effect profiles. We need to be confident that the drug has a good chance of working so that patients are not needlessly suffering.
The kind of sequencing we currently perform on DNA has been such a turning point in research that at the time of its introduction, it was called next-generation sequencing, and it still is, nearly ten years later! There are three different approaches to cancer genome applications. The first is called a targeted panel, this is when a particular set of genes that are focussed on a particular disease/cancer type are analysed. The second type is performed on a larger scale and is called Whole Exome Sequencing. In this case, all of the DNA that encodes for cellular proteins is sequenced. The third option, Whole Genome Sequencing is the most time-consuming and expensive; it sequences all the DNA present in the genome.
It has become clear that although individual genetic changes are important in matching patients to drugs, larger scale patterns of genetic changes or ‘signatures’ are also very important. These signatures are like scars in a cancer genome and record the natural history of the cancer. For example, smokers with lung cancer have a very clear signature of smoking and skin cancers have a clear Ultra-Violet light signature. Similarly, some breast cancers have a signature too, and it is likely that the presence of this signature can predict how these cancers will respond to certain drugs (e.g. cisplatin, olaparib). Importantly, in order to reliably define the signature, we need to sequence the whole cancer genome.
Can we apply this technology to breast cancers?
Around the world, leading cancer centres have begun implementing cancer genome sequencing programs and may use panels or whole exome sequencing. Some Australian doctors may send your sample to a private provider for sequencing, but it is not yet available as standard-of-care in Australia. One reason is that breast cancers are incredibly diverse. From a genomic point of view, we now think that no two breast cancers are the same. This makes it very difficult to design a small panel of relevant genes that could represent all the different kinds of changes we see in breast cancers. A small panel does not allow signatures to be analysed, which is very important in breast cancers.
What next?
We think that whole genome sequencing is crucial for precision oncology in breast cancer. Professor Sunil Lakhani and a large team of researchers and doctors from across Brisbane have been awarded funding through Queensland Genomics from Queensland Health to implement whole genome sequencing in breast cancer patients. This study is called Q-IMPROvE (IMplementation of PRecision Oncology in brEast cancer). We will take a biopsy of the cancer before the patient begins their therapy and analyse their DNA sequence. We can then advise their treating doctors about what kind of genetic changes are present, and how they would be likely to respond to different drugs. We hope to determine if whole genome sequencing is the way to innovate and future-proof breast cancer management in Australia.
Dr Amy McCart Reed
 Dr Amy McCart Reed holds a BSc (Hons) degree and a PhD in molecular biology from The University of Queensland. Her early postdoctoral work focused on understanding the genetic basis of colorectal cancer using experimental disease models, as part of a Cancer Research UK-funded colorectal cancer program.
Dr Amy McCart Reed holds a BSc (Hons) degree and a PhD in molecular biology from The University of Queensland. Her early postdoctoral work focused on understanding the genetic basis of colorectal cancer using experimental disease models, as part of a Cancer Research UK-funded colorectal cancer program.
After returning to Australia in 2009, Amy was recruited to the Molecular Breast Pathology group as a molecular genetics specialist at the UQ Centre for Clinical Research. She is passionate about clinical research and biobanking, and in addition to her breast cancer research portfolio she coordinates the Brisbane Breast Bank and the Brisbane node of the BROCADE autopsy study.
