Collection close-up archive
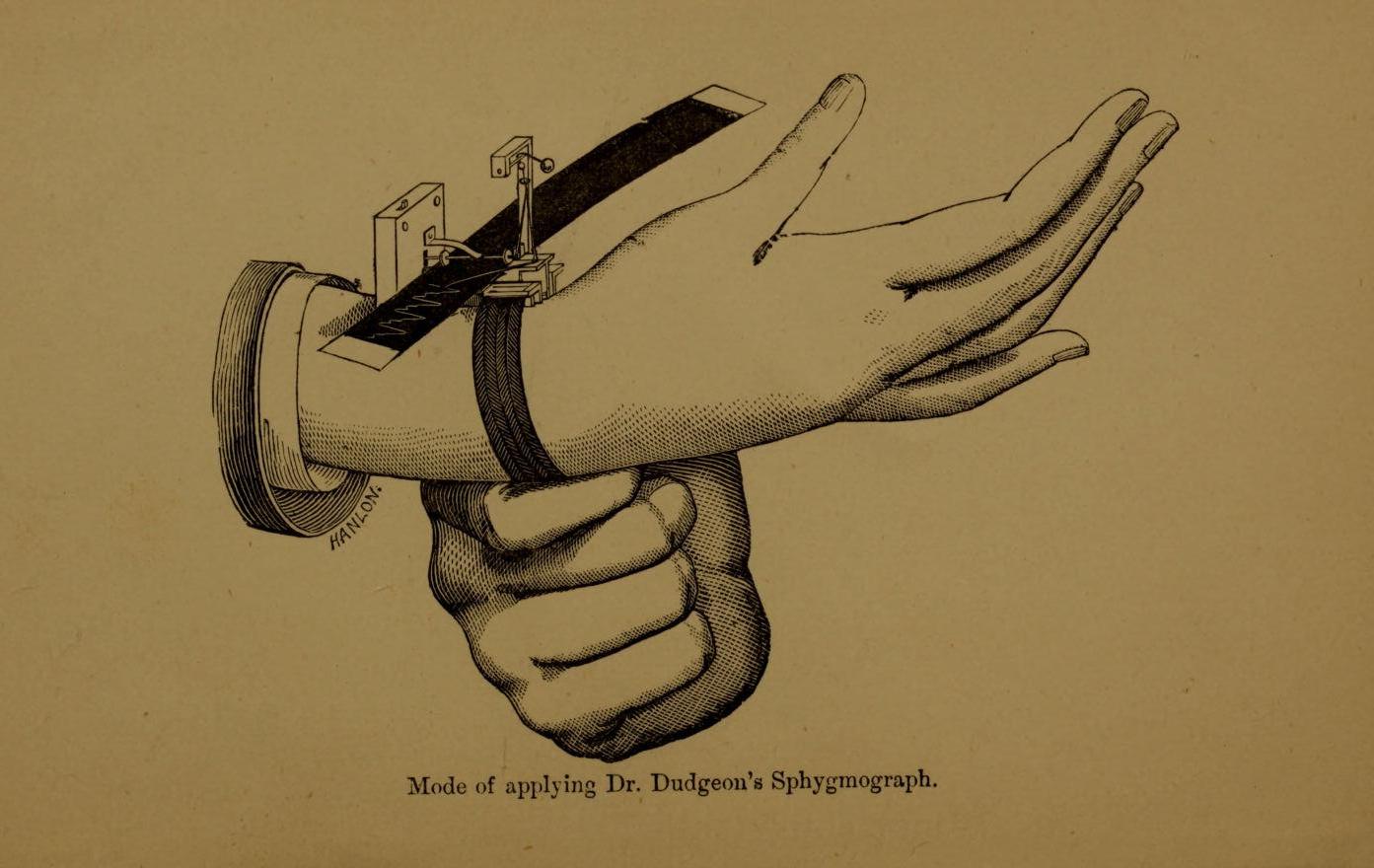
Dudgeon-type Sphygmograph, c. 1900
Dudgeon-type Sphygmograph, c. 1900
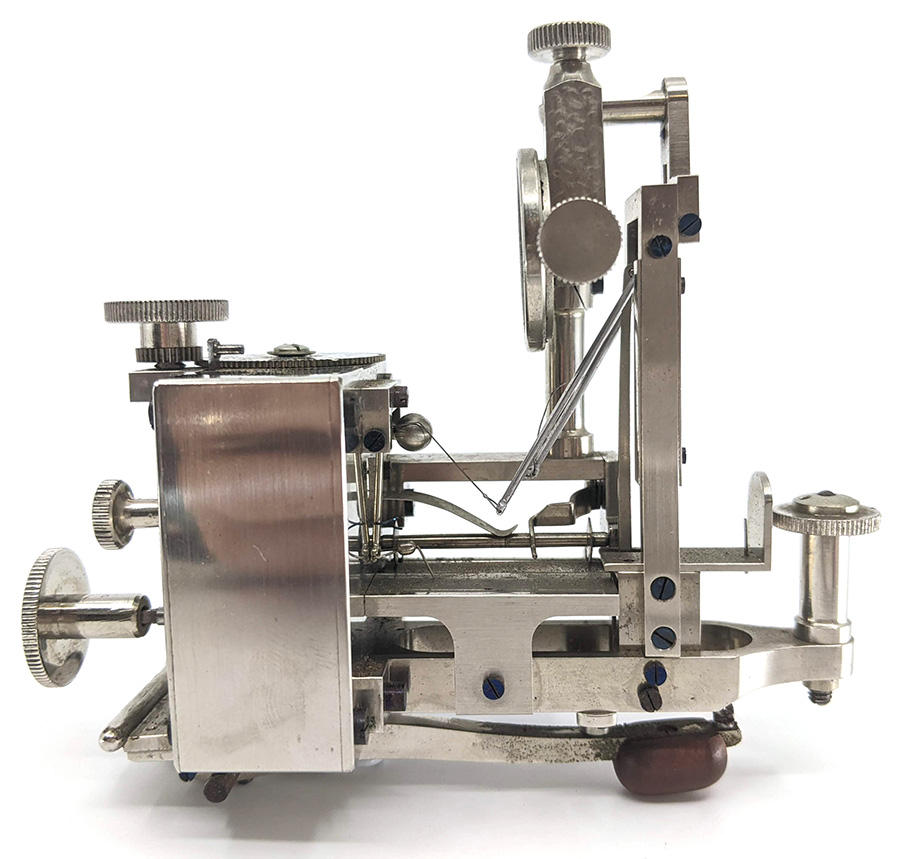 The sphygmograph is an instrument used to capture a graphic representation of the pulse. Its development was instrumental in advancing our understanding of cardiovascular physiology and was a precursor to the sphygmomanometer (blood pressure monitor) we are familiar with today.
The sphygmograph is an instrument used to capture a graphic representation of the pulse. Its development was instrumental in advancing our understanding of cardiovascular physiology and was a precursor to the sphygmomanometer (blood pressure monitor) we are familiar with today.
The instrument pictured here was strapped to the wrist with a wide ribbon or leather band, and a delicate lever on the radial artery moved a tiny stylus which recorded the pulse on smoked paper. It is an intricate, beautiful and clever piece of design.
Prior to the invention of electrocardiography, the sphygmograph was the only way to study cardiac arrhythmias and yet they were not widely adopted in clinical practice, with practitioners preferring the traditional ‘fingers on the pulse’ method. The delicate machines were difficult to use, and it took practice and training to gain an adequate pulse tracing. They were briefly embraced by the psychiatric community in the late 19th century in an attempt to ‘coax the narratives of madness from blood’. Correlations between the character of the pulse and the character of the illness were made, specifically in diagnoses of mania, melancholia and epilepsy and their subsequent response to drugs or other treatments.
The sphygmograph also enjoyed momentary fame as a lie detection device, linking emotion to blood pressure and pulse.
More about this sphygmograph can be found in the Museum’s publication “50 Treasures: a collection of objects from the Marks-Hirschfeld Museum of Medical History”.
Magneto-electric machine c. 1880
 Electricity revolutionised late Victorian society, ushering in an exciting era of electric lights, telephones and batteries. With the public fascinated by the promise and mystery of electricity, it did not take paramedicals long to capitalise on the electrical nature of animal tissue. They spruiked the logic that if a system is ‘run down’ or ‘lacking energy’, a quick application of electricity would restore vitality. This philosophy spawned a myriad of electrical belts, brushes, corsets, and this magneto-electric machine popular in the mid-late 1800s.
Electricity revolutionised late Victorian society, ushering in an exciting era of electric lights, telephones and batteries. With the public fascinated by the promise and mystery of electricity, it did not take paramedicals long to capitalise on the electrical nature of animal tissue. They spruiked the logic that if a system is ‘run down’ or ‘lacking energy’, a quick application of electricity would restore vitality. This philosophy spawned a myriad of electrical belts, brushes, corsets, and this magneto-electric machine popular in the mid-late 1800s.
The device works by rotating two solenoids (fine wires tightly wrapped around a metal core and encased in velvet) within the field of a very large magnet (blue in the photos). The spinning of the solenoids is powered by a manual crank, which generates a ‘mild’ alternating electrical current (AC) to the attached electrodes.
To use, the operator would place the electrodes in the patient’s hands or elsewhere on the patient’s body and turn the crank. The faster it was turned, the greater the current. The makers claimed that it could relieve pain, as well as cure numerous diseases, including cancer, tuberculosis, diabetes, gangrene, heart disease, tetanus, and spinal deformities.
The Museum is lucky to have two of these objects in excellent, presumably working, condition in its collection.

Ergot Aseptic c. 1920
Ergot has been used for centuries to hasten childbirth by causing violent contractions of the uterus. One hundred years ago, ampoules of ergo aseptic like these were a common intravenous treatment for postpartum haemorrhage.
Ergot is a fungus that attacks rye and can be extremely toxic. It contains lysergic acid, from which LSD is derived. Long-term ergot poisoning, or ergotism, causes psychosis, mania, blood constriction, hallucinations and seizures.
Epidemics of the disease have been identified throughout history. Being impervious to heat and water, the toxic properties of ergo could survive being baked into rye bread, and tainted crops could affect entire communities. There was no known cure for ergotism, nor was there knowledge of the source of the poison. As rye bread was a staple food in many parts of Europe and America, sufferers of ergotism would often continue to imbibe ergot-laden food. The resulting vasoconstriction would cause dry gangrene, oedema and ultimately the loss of limbs.
Ergo-induced hysteria has been put forward as a theory behind the ‘bewitchment’ that spurred the Salem witch in 1692. In France it has been linked to the Dancing plague of 1518 and the Great Fear of 1789 at the start of the French Revolution.
Junker’s inhaler
Chloroform was discovered at around the same time as Morton’s demonstration of the anaesthetic effects of ether in 1847. Initially, the vapours were inhaled from a handkerchief or piece of lint held over the patient’s face, but both substances were found to damage the skin so various wire frames were made to prevent this happening. Droppers were used to administer the ansaesthetic - the patient breathed the vapour of liquid chloroform dropped onto the fabric of the mask (the ‘draw-over’ method).
Dr Ferdinand E. Junker was an Austrian who had worked in Germany, Japan and England. In 1860, Junker devised a system where chloroform vapour could be administered directly to the mask without using the dropper method (the ‘blow-over’ method). A rubber bellows similar to those used on the everyday sphygmomanometer was used to pump air which had passed over chloroform in the bottom of a glass container into the inspiratory limb and directly to the patient’s mask. Both limbs were labelled. The inhaler has a hook so that it could be suspended around the neck of the anaesthetist, keeping it in a vertical position and preventing liquid chloroform from running directly into the mask. Despite various modifications to prevent it, the concentration of agent reaching the patient was difficult to quantitate and would quite often be excessive.
The Museum currently has a display on the development of ether, which can be seen on level 3 of the Mayne Medical Building.

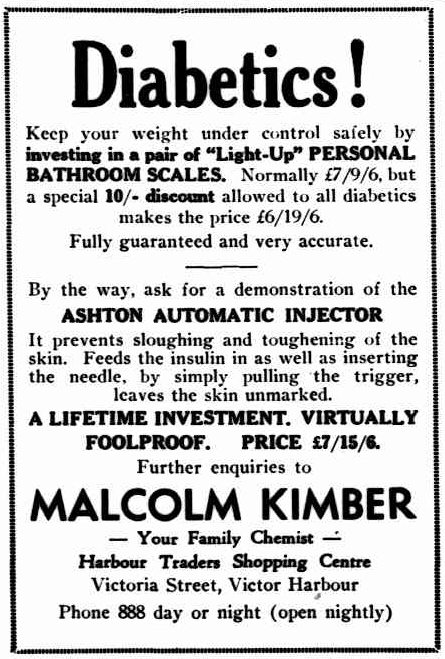
Ashton automatic injector
The Ashton automatic injector was developed in the 1950s for patients who were apprehensive to self-inject. Many were diabetics who required several daily injections.
The device was spring-loaded with a Luer lock syringe and needle, filled with the appropriate dose of insulin. A patient would hold the injector firmly against the skin and squeeze the trigger, injecting the needle to the depth of the hypodermis. The maker claimed that the procedure was almost painless.
It was invented and designed by Mr. Donald Lewis of Port Lincoln, and manufactured by Ashton & Co. Ltd in Hilton, South Australia. Problems with bacterial contamination and proper sterilisation meant the automatic injector had a limited production life.
The Marks-Hirschfeld Museum collection includes three Ashton automatic injectors, two of which are in their original boxes with instruction manuals.

Dr Petz’ stomach stapler
The first surgical stapler was developed in 1908 by Dr Húmer Hültl in Hungary. While it worked well and was a revolution in stomach surgery, it was heavy, cumbersome and expensive. Surgeons were reticent to adapt to this new technology.
In 1920 another Hungarian, Dr Aladár Petz improved on the original stapler by making it lighter, easier to use and more affordable. The Von Petz stapler in the Marks-Hirschfeld Museum collection is a model that was adopted all over the world and was in use until the early 1970s. This stapler is in excellent condition and includes the original silver staples that were used with this machine.

The Museum holds an extensive collection of surgical equipment, with many objects that demonstrate the evolution of surgical technology and innovation.
“I designed the gastro-intestinal suturing instrument in 1920 while working as an assistant professor. The idea stemmed from the need that the surgeon has to open the digestive tract with its highly contaminated lumen, there-by, risking consequent peritonitis with its associated in-crease in mortality. Simple manual suturing of the infected lumen of the intestine is time consuming, thus pro-longing surgery and increasing the risk of mortality for patients under anaesthesia.’
Dr Aladár Petz
